Warren and Patsy Nelms are both 83-year-old residents of Oak Hammock, a Gainesville retirement and assisted-living community. After more than 50 years of living together, they now live separately — Patsy in an independent home and Warren, who has dementia, in assisted care.
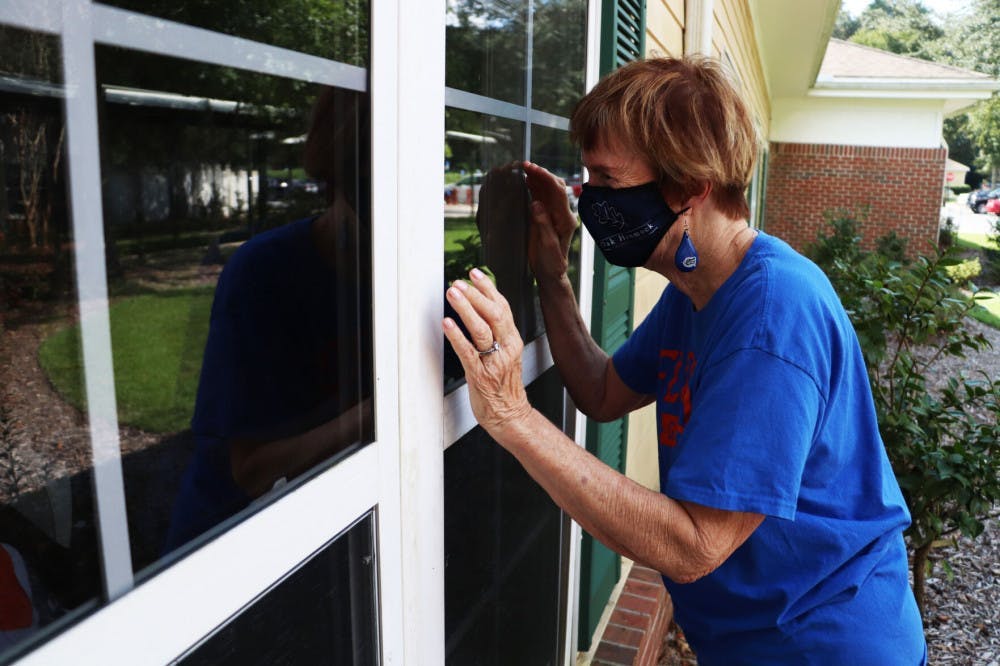
She parks her golf cart — clad in Gator bumper stickers — outside Oak Hammock’s health pavilion, where a nurse feeds Warren his meals. Patsy walks across the health pavilion’s lawn and stands by the window, waving at Warren as he enjoys his pre-mushed meat and potatoes. During these window visits, his reactions are limited.
Life in retirement and long-term care facilities has been drastically uprooted by the COVID-19 pandemic. Windows and plexiglass now separate spouses and families, leaving the population’s most mentally vulnerable to battle the anxiety of a pandemic that has killed thousands of Florida’s seniors.
But the effects of the pandemic reach beyond the lives it has taken — loneliness, delirium and mental decline also threaten seniors in isolation.
In Florida, people 65 years or older have accounted for 52% of hospitalizations and 82% of deaths, according to the Florida Department of Health’s most recent COVID-19 report.
Despite this population being at high risk, long-term care facilities and nursing homes are slowly reopening across the state.
Thursday, Florida Gov. Ron DeSantis directed the Florida Division of Emergency Management to allow children to visit long-term care facilities, remove a five-person maximum visitation policy, and limit restrictions on outdoor visitation.
Florida has had over 775,000 COVID-19 cases — the third highest out of all states — and about 16,500 people have died. About 50,000 cases and 6,000 deaths have occurred in Florida’s long-term care facilities.
With restrictions being lifted, seniors in assisted living now have more opportunities to visit loved ones.
Patsy and Warren
Oak Hammock’s nurses know to feed Warren by a particular window so he and Patsy can see each other every day.
After spending a few minutes with Warren, she headed back home, puttering through the Oak Hammock streets in her golf cart. “G8R FAN,” the license plate read — Patsy and her husband are both 1959 UF alumni. They married a year before they graduated.
Oak Hammock resembles any regular suburban neighborhood: The independent living section is made up of five-story apartment buildings and houses on winding roads. The community feels otherworldly, tucked away in the greenery of moss-riddled oak trees.
Patsy and Warren moved to Oak Hammock together in 2013, opting to live in a house surrounded by a lush garden where purple flowers dangle from trees and hummingbirds whiz about.
About 15 years ago, Warren began having memory difficulties. When they lived together at Oak Hammock, Patsy said he began falling, and he would sometimes have trouble getting back up. She knew he would have to be moved into assisted living, where nurses could provide him with 24-hour care.
About two years ago, he was moved to memory care, a facility that provides specialized care for those with Alzheimer's or dementia. Patsy was able to visit him at any time. They would sing together, Warren often leading them in songs like “You Are My Sunshine.”
But Warren’s physical and mental capabilities continued to decline. This year, he lost his ability to communicate.
Before the pandemic, he was moved to the skilled nursing unit, where nurses help him with everyday tasks. Patsy said residents are sent there when they can’t get out of bed on their own.
But she said he’ll sometimes smile at her, and he doesn’t give the nurses a hard time.
“He’s lasted way longer than they expected him to,” Patsy said. “He’s not unhappy, and he’s not suffering.”
During the summer — the height of the pandemic — visitation and social restrictions in the community were more firm. Dining facilities were closed, in-person activities were canceled and residents were encouraged to isolate.
Residents in assisted living had the most restrictions, said Katherine Osman, Oak Hammock’s director of community affairs. She said nobody could come inside to visit them, including spouses and other family.
“A lot of these people chose Oak Hammock because a spouse needed extra care and they wanted to be under the same roof with them,” Osman said. “And to be separated — it's tough.”
In April, 12 Oak Hammock residents and staff tested positive for COVID-19. As of Friday, there are no active cases among Oak Hammock residents, but two active cases among staff.
One Oak Hammock resident died of COVID-19, according to the Florida Department of Health’s report on deaths in long-term care facilities.
Osman said some independent-living residents still spend most of their time in isolation.
The staff developed a strategy to keep tabs on those in independent living. Residents place sticky notes on the outside of their doors if they are doing well; staff checked residents’ doors every morning and called those who didn’t display the signal.
She said only a few residents still participate in the daily sticky-note-check-ins — mainly those who live alone and enjoy receiving the call.
Normally, Patsy is active in the community: chamber music group, book club, pilates, coeditor of the community’s newsletter, “The Oak Leaf.”
Recently, the paper published a compilation of residents’ miniature pandemic memoirs, inspired by a similar piece in The New York Times.
“In pandemic’s throes, my garden grows!” read Patsy’s memoir.
“Home sweet home! Secret introvert guilt,” wrote one resident.
“So many lost. So much missed,” wrote another.
DeSantis and the Florida Division of Emergency Management began lifting visitation restrictions in early September, allowing entry for family and friends if they wore personal protective equipment.
Since then, active cases have declined among the state’s long-term care residents, according to the Florida Department of Health. As of Saturday, there were 859 active cases — down from about 2,000 a month ago. But, cases have remained relatively consistent among long-term care facility staff. A month ago, there were about 3,000 active cases; as of Saturday, there were more than 2,200.
With the recently lowered restrictions — Oak Hammock now allows entry for outside visitors — Patsy occasionally invites friends to sit on her porch and share her homemade, frosty peppermint ice cream — a Patsy Nelms staple, which she offers within minutes of entering her home.
Dozens of homemade books, calendars and photo albums are stacked around her house, each containing collages of family events.
A book titled “Growing Up” displays her and Warren, decades ago, sitting on a swing set with their two children. Many document vacations at Bird Island — a special place for Patsy.
Aside from countless family outings, it’s also the site of a UF archaeological dig she participated in — where she, of course, served peppermint ice cream to all the excavators — and it’s even where she and Warren had their honeymoon.
Lately, Patsy has been able to visit with Warren on a bench outside the health pavilion. She sings to him.
“He used to always be the one that would lead singing,” she said.
She sings him a variation of “Old Folks at Home,” or “Suwannee River,” which they would sing as they drove over the river on their trips to Bird Island.
“Not so far above the Suwannee River lies our island home, bright and shining in the blue Gulf waters, to it we love to roam.”
“Delirium Prevention Champions”
In hospitals, COVID-19 patients face the threat of delirium: a state of mental confusion and disorientation.
It’s a symptom of COVID-19 doctors weren’t ready to combat when the pandemic spread throughout the U.S. in March. Since then, doctors at UF Health have worked to prevent it through “Delirium Prevention Champions,” a program where nurses suit up in PPE to reorient COVID-19 patients by spending time with them.
Delirium can manifest in several ways beyond disorientation and confusion, said Dr. Mariam Mufti, a UF assistant professor in geriatric medicine. She said it can cause behavioral responses, including agitation, hallucinations, hitting and spitting.
“It's very difficult to orient someone… when they're isolated in a room and have some underlying dementia and infection going,” Mufti said. “That was one of many things that we saw.”
Dementia can exacerbate the effects of delirium, because when a patient already has limited cognitive function, it becomes harder to reorient them, said Dr. Nila Radhakrishnan, chief of the division of hospital medicine and director of UF Health’s Delirium Champions Program.
She said the best way to prevent it involves physically interacting with people, which proved difficult when patients were suffering from a contagious virus.
The solution: delirium prevention champions, nurses in head-to-toe in PPE who spend time with patients. This involves physical touch, conversations, activities and coordinating video chats with family.
One of the delirium prevention champions, nurse Jennifer Melara, said she was anxious about interacting with COVID-19-positive patients at first.
“But certainly once we got in the rooms, you could definitely see the need for the patient to have more interaction with people,” she said.
Melara and the other nurses visited between 15 and 25 people a day from a few minutes to an hour, she said.
“Some patients had limited ability to carry a conversation,” Melara said. “Others could tell you their whole life story.”
Aside from conversation, the nurses offered games and art activities for further cognitive stimulation. They offered coloring, painting, virtual music therapy and puzzles, depending on the patient’s preferences.
Suzanne Maye, another delirium champion nurse, said she cared for a patient with cognitive levels similar to those of dementia. The patient was often confused and agitated, and she even had to be restrained because she was hitting staff.
Maye said she coordinated virtual visitation with the patient’s family, which helped her communicate with the patient to fulfill her needs. They took her off restraints, and at one point, the patient’s family called Maye a part of their family.
"That was one of the most heartwarming interactions I've had,” she said.
Delirium can have a negative impact on a patient’s future cognitive abilities, said Catherine Price, a neuropsychologist and assistant professor at UF. She said individuals who have developed delirium have a higher rate of cognitive decline over time as well as a higher mortality rate.
“Intervening on delirium is truly vital to a patient's long-term outcome,” Price said.
Valerie Griffith
In the pandemic’s seven months of isolation, Valerie Griffith’s friend has experienced six years’ worth of mental decline.
Griffith, 80, has been a resident of Oak Hammock for 16 years; for as long as the community has been open, she’s lived there. She moved there alone after her husband’s ten-year fight with dementia. He lived in a nursing home for the last six years of his life.
After living at Oak Hammock for seven years, Griffith received a call from an old friend from college — both of them UF alumni. He subsequently moved there, and after a 45-year break in their relationship, they reunited.
He was moved to assisted living after he started forgetting to take his medication. But other than that, Griffith said he was mostly fine; he took care of himself, enjoyed his usual activities, and continued meeting her for dinner.
But the pandemic separated them.
By May, he was moved into memory care, where residents were restricted from having visitors. Five months later, Griffith said he has difficulty bathing and dressing himself, and he has trouble holding a coherent conversation.
“It’s the isolation,” she said. “It’s unbelievable. It’s very destructive to people who have any kind of mental problems.”
She said his long-term memory persists, because he recalls their years in college together — occasionally, he has moments of lucidity. But in just seven months of isolation, she said he’s had a similar level of mental decline as her husband’s six years in a nursing home.
Griffith said it’s been a huge loss for her and Oak Hammock. Because of his sociable nature, she said he was loved among the entire community.
“We had hoped that he would be at least marginally able to exist,” she said. “But not anymore. He’s not going to ever come back.”
But Griffith said she’s doing OK, because she can tell he’s happy. He’s told her that he enjoys living in the memory unit; he loves the food, and he likes talking to the nurses.
Depending on the conditions of a person’s isolation, a lack of stimulation can have negative effects on a person’s cognition, said UF neuropsychologist Catherine Price.
She described the brain as a “sensory input system” that needs cognitive stimulation to remain healthy. She said this comes in a variety of forms, including stimulating all five senses and fostering different types of social interaction.
Interaction with lifelong friends and family triggers different neurons and blood flow compared to interaction with strangers.
“When you're with somebody that you know, there's a kindling of old memories,” Price said. Regardless of whether a person has dementia or COVID-19-induced delirium, Price said isolation can cause depression, anxiety and loneliness.
Griffith said the pandemic has instilled a fear and frustration in her she’s never experienced. “It’s because I’m 80, and now I’m like, ‘OK, I don’t have that many years left,’” she said. “I don’t want to mess it up.”
Monica Ondrick, social services liaison at Oak Hammock, said the staff has been working hard to keep assisted-living residents engaged to try to stave off the harmful effects of isolation.
“The staff has put a lot of things in place to help try to combat some of the depression and the sadness that has come from people not seeing their families,” she said.
Ondrick said assisted-living staff offers daily FaceTime opportunities for residents to video chat with family, and the staff even puts on shows to brighten the residents’ days.
On Fridays, staff line dances down the halls of the assisted-living facility, and residents dance and clap along in their doorways. One week, a staff member wore a blow-up dinosaur costume, which Ondrick said brought smiles to the residents’ faces.
She said visitation restrictions have lessened, so people in assisted living are able to spend time with visitors outdoors — as long as they’re wearing PPE.
Griffith has visited her friend several times since restrictions were lifted. She said she’s allowed to visit him twice a week, but she calls him every day. She said the five- to 10-minute conversations are disjointed.
During in-person visits, Griffith is required to wear full PPE, including an N95 mask, and head and body coverings. She said sitting next to him in complete protective gear feels odd, but he doesn’t seem to mind. He also wears a mask.
They sit in one of Oak Hammock’s courtyards and talk, separated six feet apart. Because his long-term memory is functional, she said he’ll sometimes talk about his life: the friends, places and memories from the 45-year gap she wasn’t a part of.
But other times, he’ll recall memories from their college years.
Griffith feels he isn’t getting enough mental stimulation, because at the beginning of their talks, he’s usually disoriented. By the end, she said he’s much more aware of his surroundings.
“You can't expect staff to give them the time that you’d give them as an individual,” she said.
She said she wishes restrictions would be lifted even more, at least to allow a few close family members to spend more time with people in assisted living.
“Is it better that he's mentally gone, as opposed to being physically gone?” Griffith said.
Contact Thomas Weber at tweber@alligator.org. Follow him on Twitter @thomasjohnweber.